Cardiovascular effects
Cardiovascular effects are defined as any uncomfortable physical effect which relates to the heart and blood vessels.
This page lists and describes the various cardiovascular effects which can occur under the influence of certain psychoactive compounds.
Abnormal heartbeat
Abnormal heartbeat (also called an arrhythmia or dysrhythmia) is defined as a problem with the rate or rhythm of a heartbeat.[1] A heartbeat that is too fast (greater than 100 beats per minute) is called tachycardia and a heartbeat that is too slow (less than 60 beats per minute) is called bradycardia. Arrhythmias are caused by changes to heart tissue. Hearts beat due to cascading electrical signals and these can be influenced by stress hormones, electrolytes, and medicinal substances.
An abnormal heartbeat is most commonly induced under the influence of moderate dosages of stimulant and depressant compounds, such as cocaine,[2][3][4][5][6][7][8] amphetamines,[9][10][11][12][13] alcohol,[13] and opioids.[13][14][15] While stimulants tend to increase a person's heart rate, depressants tend to decrease it. Combining the two can often result in dangerously irregular heartbeats.
Decreased blood pressure
Decreased blood pressure can be described as a condition in which the pressure in the systemic arteries is decreased to abnormal levels. A blood pressure of 120/80 is considered normal for an adult. A blood pressure of 90/60 or lower is considered hypotension and a blood pressure between 120/80 and 90/60 is considered prehypotension.[16]
Decreased blood pressure is most commonly induced under the influence of moderate dosages of GABAergic depressant compounds, such as benzodiazepines and barbiturates. However, it can also occur under the influence of vasodilating compounds such as poppers as well as certain psychedelics and stimulants in an unpredictable manner.
Decreased heart rate
Decreased heart rate or bradycardia can be described as a heart rate that is lower than the normal heart rate at rest. The average healthy human heart normally beats 60 to 100 times a minute when a person is at rest. When the heart rate fluctuates to lower levels under 60 BPM, it is described as bradycardia or an abnormally low heart rate.
It is worth noting that decreased heart rate can often be a result of psychological symptoms as a natural response to relaxation, anxiety suppression, sedation, and mindfulness.
Decreased heart rate is most commonly induced under the influence of heavy dosages of depressant compounds, such as GABAergics, and opioids. However, it can also occur under the influence of cannabinoids, dissociatives, and stimulants.
Increased blood pressure
Increased blood pressure can be described as a condition in which the pressure in the systemic arteries is elevated to abnormal levels. A blood pressure of 120/80 is considered normal for an adult. A blood pressure of 90/60 or lower is considered hypotension and a blood pressure between 120/80 and 90/60 is considered prehypotension.[17] Conversely a blood pressure greater than 120/80 and less than 139/89 is considered prehypertension.
Within the medical literature, a situation in which a person's blood pressure is very high (e.g., >180/>110 mmHg) with minimal or no symptoms, and no signs or symptoms indicating acute organ damage is referred to as a "hypertensive urgency".[18] In contrast, a situation where severe blood pressure is accompanied by evidence of progressive organ or system damage is referred to as a "hypertensive emergency".
Increased blood pressure is most commonly induced under the influence of heavy dosages of vasoconstricting compounds, such as traditional stimulants and stimulating psychedelics.
Increased heart rate
Increased heart rate or tachycardia is described as a heart rate that is faster than the normal heart rate at rest. The average healthy human heart normally beats 60 to 100 times a minute when a person is at rest. When the heart rate fluctuates to higher levels over 100 BPM, it is described as tachycardia or an abnormally high heart rate.
It is worth noting that increased heart rate can often be a result of psychological symptoms as a natural adrenal response to anxiety, paranoia, shock, and fear.
Increased heart rate is most commonly induced under the influence of heavy dosages of stimulating compounds, such as traditional stimulants, certain psychedelics, and certain dissociatives. This is thought to occur as a direct result of dopaminergic or adrenergic modulation.[19][20] However, it can also occur under the influence of deliriants due to the way in which they inhibit acetylcholine, one of the main modulaters of heart rate in the peripheral nervous system.[21][22]
Vasoconstriction
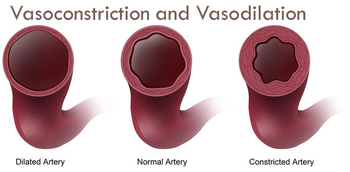
Vasoconstriction can be described as a narrowing of the veins and blood vessels which results from a contraction of their muscular wall. It is particularly prevalent in the large arteries and small arterioles.
This effect typically results in feelings of tightness, achiness, and numbness within a person's arms and legs. It can range from mild in its effects to extremely uncomfortable.
Vasoconstriction is often accompanied by other coinciding effects such as stimulation. It is most commonly induced under the influence of moderate dosages of stimulating psychedelic compounds, such as LSD, 2C-E, and DOC. However, it can also occur under the influence of traditional stimulants such as methamphetamine, caffeine, and MDMA.
Vasodilation
Vasodilation can be described as a widening of the veins and blood vessels which results from the relaxation of smooth muscle cells within the vessel walls. It is particularly prevalent in the large arteries and small arterioles. The primary function of vasodilation is to increase blood flow in the body to tissues that need it most. In essence, this process is the opposite of vasoconstriction, which is the narrowing of blood vessels.
This effect is typically very difficult to consciously perceive but often results in a bloodshot red eye effect and relief from glaucoma.
Vasodilation is often accompanied by other coinciding effects such as decreased blood pressure. It is most commonly induced under the influence of moderate dosages of cannabinoid compounds, such as cannabis, JWH-018, and THJ-018. However, it can also occur under the influence of poppers and viagra.
See also
References
- ↑ Arrhythmias - What Is an Arrhythmia?, National Heart, Lung and Blood Institute, retrieved 4 June 2022
- ↑ Wood, D. M., Dargan, P. I., Hoffman, R. S. (January 2009). "Management of cocaine-induced cardiac arrhythmias due to cardiac ion channel dysfunction". Clinical Toxicology. 47 (1): 14–23. doi:10.1080/15563650802339373. ISSN 1556-3650.
- ↑ O’Leary, M. E., Hancox, J. C. (28 January 2010). "Role of voltage-gated sodium, potassium and calcium channels in the development of cocaine-associated cardiac arrhythmias: Voltage-gated ion channels and cocaine-induced arrhythmia". British Journal of Clinical Pharmacology. 69 (5): 427–442. doi:10.1111/j.1365-2125.2010.03629.x. ISSN 0306-5251.
- ↑ Wood, D. M., Dargan, P. I. (28 January 2010). "Putting cocaine use and cocaine-associated cardiac arrhythmias into epidemiological and clinical perspective: Cocaine epidemiology and cardiovascular toxicity". British Journal of Clinical Pharmacology. 69 (5): 443–447. doi:10.1111/j.1365-2125.2010.03630.x. ISSN 0306-5251.
- ↑ Gradman, A. H. (April 1988). "Cardiac effects of cocaine: a review". The Yale Journal of Biology and Medicine. 61 (2): 137–147. ISSN 0044-0086.
- ↑ Lange, R. A., Hillis, L. D. (2 August 2001). "Cardiovascular Complications of Cocaine Use". New England Journal of Medicine. 345 (5): 351–358. doi:10.1056/NEJM200108023450507. ISSN 0028-4793.
- ↑ Tazelaar, H. D., Karch, S. B., Stephens, B. G., Billingham, M. E. (February 1987). "Cocaine and the heart". Human Pathology. 18 (2): 195–199. doi:10.1016/S0046-8177(87)80338-6. ISSN 0046-8177.
- ↑ Maraj, S., Figueredo, V. M., Lynn Morris, D. (May 2010). "Cocaine and the Heart". Clinical Cardiology. 33 (5): 264–269. doi:10.1002/clc.20746. ISSN 0160-9289.
- ↑ Shyu, K., Wang, B., Yang, Y., Tsai, S., Lin, S., Lee, C. (1 July 2004). "Amphetamine activates connexin43 gene expression in cultured neonatal rat cardiomyocytes through JNK and AP-1 pathway". Cardiovascular Research. 63 (1): 98–108. doi:10.1016/j.cardiores.2004.02.018. ISSN 0008-6363.
- ↑ Bazmi, E., Mousavi, F., Giahchin, L., Mokhtari, T., Behnoush, B. (30 March 2017). "Cardiovascular Complications of Acute Amphetamine Abuse: Cross-sectional study". Sultan Qaboos University Medical Journal. 17 (1): e31–37. doi:10.18295/squmj.2016.17.01.007. ISSN 2075-051X.
- ↑ Jacobs, W. (June 2006). "Fatal Amphetamine-Associated Cardiotoxicity and Its Medicolegal Implications:". The American Journal of Forensic Medicine and Pathology. 27 (2): 156–160. doi:10.1097/01.paf.0000188082.68009.10. ISSN 0195-7910.
- ↑ Won, S., Hong, R. A., Shohet, R. V., Seto, T. B., Parikh, N. I. (December 2013). "Methamphetamine-Associated Cardiomyopathy: Methamphetamine-associated cardiomyopathy". Clinical Cardiology. 36 (12): 737–742. doi:10.1002/clc.22195. ISSN 0160-9289.
- ↑ 13.0 13.1 13.2 Frishman, W. H., Del Vecchio, A., Sanal, S., Ismail, A. (July 2003). "Cardiovascular Manifestations of Substance Abuse: Part 2: Alcohol, Amphetamines, Heroin, Cannabis, and Caffeine". Heart Disease. 5 (4): 253–271. doi:10.1097/01.hdx.0000080713.09303.a6. ISSN 1521-737X.
- ↑ Behzadi, M., Joukar, S., Beik, A. (2018). "Opioids and Cardiac Arrhythmia: A Literature Review". Medical Principles and Practice. 27 (5): 401–414. doi:10.1159/000492616. ISSN 1011-7571.
- ↑ Doshi, R., Shah, J., Desai, R., Gullapalli, N. (July 2019). "Burden of arrhythmia in hospitalizations with opioid overdose". International Journal of Cardiology. 286: 73–75. doi:10.1016/j.ijcard.2019.01.047. ISSN 0167-5273.
- ↑ Low Blood Pressure - NHLBI, NIH, retrieved 4 June 2022
- ↑ Low Blood Pressure - NHLBI, NIH, retrieved 4 June 2022
- ↑ Pak, K. J., Hu, T., Fee, C., Wang, R., Smith, M., Bazzano, L. A. (2014). "Acute hypertension: a systematic review and appraisal of guidelines". The Ochsner Journal. 14 (4): 655–663. ISSN 1524-5012.
- ↑ Billman, G. E. (May 1990). "Mechanisms responsible for the cardiotoxic effects of cocaine". The FASEB Journal. 4 (8): 2469–2475. doi:10.1096/fasebj.4.8.2185973. ISSN 0892-6638.
- ↑ Ferreira, M. T., Ferreira, R., Carvalho, F., Duarte, J. A. (1 November 2006). "Effect of physical exercise on markers of acute cardiotoxicity induced by d-amphetamine in an animal model". Revista portuguesa de cardiologia. 25 (11): 983–996. ISSN 2174-2030.
- ↑ Triposkiadis, F., Karayannis, G., Giamouzis, G., Skoularigis, J., Louridas, G., Butler, J. (November 2009). "The Sympathetic Nervous System in Heart Failure". Journal of the American College of Cardiology. 54 (19): 1747–1762. doi:10.1016/j.jacc.2009.05.015. ISSN 0735-1097.
- ↑ Akselrod, S., Gordon, D., Ubel, F. A., Shannon, D. C., Berger, A. C., Cohen, R. J. (10 July 1981). "Power Spectrum Analysis of Heart Rate Fluctuation: A Quantitative Probe of Beat-to-Beat Cardiovascular Control". Science. 213 (4504): 220–222. doi:10.1126/science.6166045. ISSN 0036-8075.